Weston County Manor nears its mark
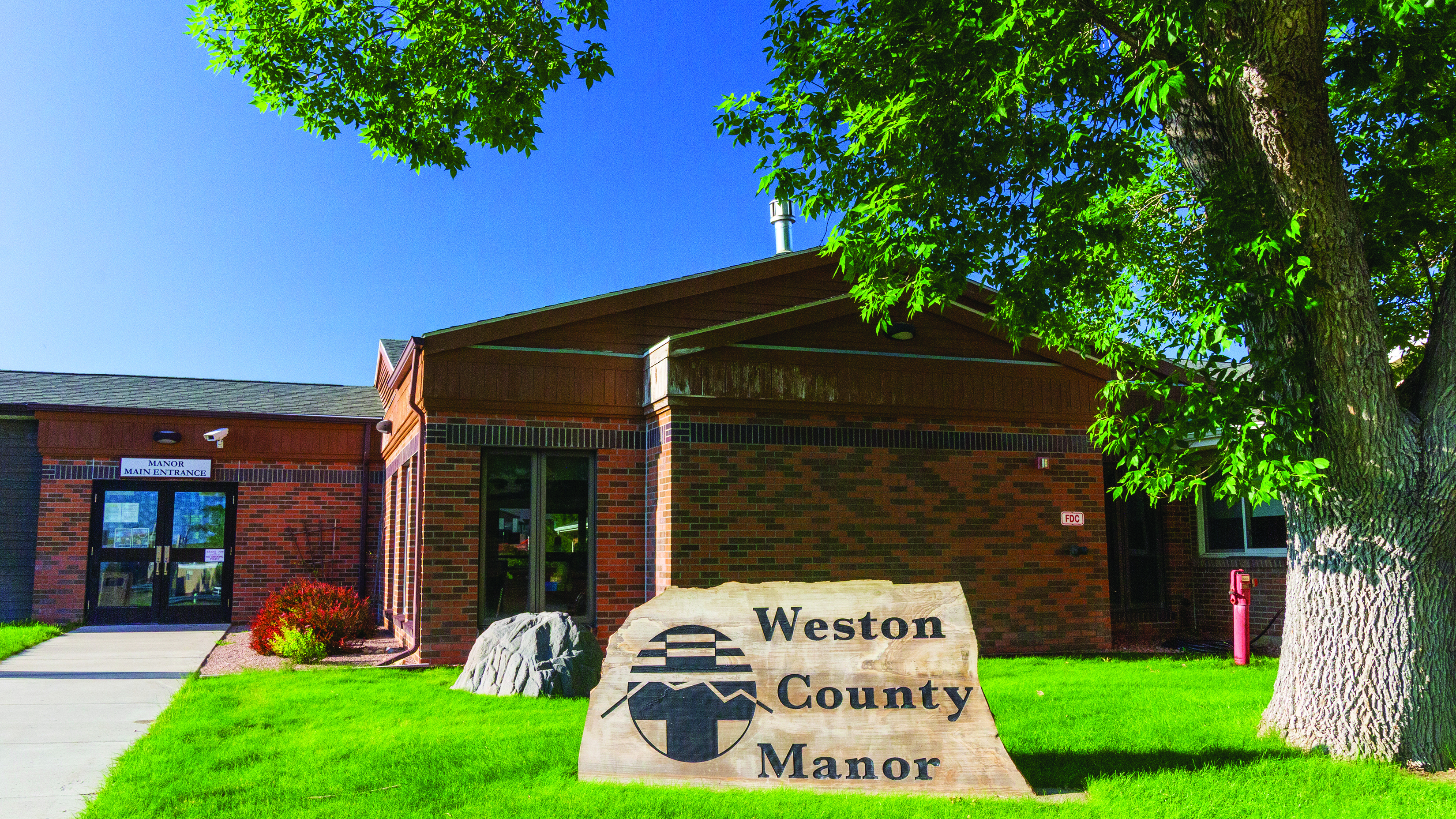
Photo by Amy Menerey/NLJ Weston County Manor, the long-term nursing home facility at Weston County Health Services, has reached its break-even point financially.
Weston County Health Services’ nursing home has at last reached its break-even point financially, according to Weston County Hospital District trustee Nathan Ballard, who serves on the board’s finance committee.
Previously, the hospital was losing a lot of money just through the Weston County Manor, according to Ballard, and one problem was that not enough of the facility’s 58 beds were filled.
John Gantner, the former interim chief financial officer, estimated several months ago that the hospital would lose $1 million a year with the nursing home resident count at just 40, and the financial needs of that part of the facility are pressing. The Manor needs about $2 million to upgrade the heating, ventilating and air conditioning system, according to Ballard.
Shane Filipi, the nursing home’s administrator, told the News Letter Journal that the Manor’s population, currently at 46, was in the 50s before the COVID-19 pandemic. From what he can recall, its population was in the mid-30s in summer 2024, and when he began working for the hospital in August, the population was 37.
“No money, no mission, as they say, so we were at a very dangerous place with 40,” Ballard told the NLJ.
The hospital lost $2.36 million according to the fiscal 2023 audit report. Ballard said at the Feb. 22 board meeting that he anticipates there will also be a loss for fiscal 2024, and so far, based on cash reports, the hospital is also losing money in fiscal 2025.
Both Ballard and Filipi want to see the population back in the 50s, and they’re close to hitting that mark.
“We actually have six referrals we’re looking at, so I think that number’s probably pretty attainable,” Filipi said, noting that people are in need of nursing home services.
He said that getting the word out about the Manor and following up when prospective residents call has been important.
“At one point, people thought we were full, and we weren’t,” Ballard agreed.
Ballard explained that it had troubled him how the Manor, which he sees as “maybe the nicest ‘manor’ around,” wasn’t anywhere near full. When he asked community members why they believed the Manor didn’t have more residents, they told him that they had believed it was full. They believed that when hospital leadership discussed “swing beds,” that meant that the Manor had a waiting list. Instead, swing beds refer to short-term patient stays in the nursing home. Typically, swing-bed patients are recuperating from surgeries and no longer need to stay at larger facilities, such as Campbell County Health in Gillette.
Ballard and Filipi believe an upcoming marketing video that will highlight the Manor’s features should help, and Filipi said he anticipates the video will come out in the next month. It will showcase to prospective residents’ family members what the facility offers. It will be particularly helpful for families who don’t live nearby.
“Everybody wants to know where their loved one may be going,” Filipi said.
Ballard said another one of the issues was that the Manor was accumulating the largest portion of the overall overtime “some months ago.” The Manor is now using fewer contract certified nursing assistants, and the hospital is starting its own CNA program, which is largely online training, he said.
According to Ballard, it took both better communication and better management to accomplish the increase in occupancy. Filipi was instrumental in the changes, but Filipi said he’s grateful to staff members for all their hard work.
Ballard credits CEO Cathy Harshbarger with hiring Filipi and Filipi’s ability to focus on and fix the Manor’s problems to turn things around. He sees Filipi as one of the strong leaders the hospital is building within its system, and indicated that the level of employee supervision has improved since he came on board.
Ballard said that Filipi noticed that certain Manor staff were exploiting the hospital, Ballard said.
“There have been people who just want to take, and they don’t care if they hurt our community and hurt our hospital,” Ballard said.
There’s now been a cultural shift that is making that mentality untenable, according to Ballard.
Ballard said that when he, as a member of the board’s search committee for candidates for the position, reviewed Filipi’s resume, he perceived that the administrator had talents when it came to solving problems with people, money and facilities. While there were some concerns about the expense of having a full-time administrator, “the math was pretty simple,” Ballard said.
“If Shane can come in and make a lot of improvements, and if we can pick up two more patients a month, then he’s more than paid for himself,” he said.
The beds-filled count isn’t the only number that has improved, he noted. The Manor’s Medicare star rating has improved too. In June 2024, when Harshbarger began working for the hospital, the Manor’s star rating was one out of a possible five, according to Ballard. Now, it’s three, though he believes the care is better than three.
“There is a time delay from when quality improves to when Medicare will measure and report the improvement,” he said.
Ballard said the hospital expects to reach five out of five stars in the next few quarters.
“This was a big win for the community,” Ballard said, noting that the hospital’s focus will now shift to improvements at the clinic.
Ballard said that the change at the Manor is a bigger achievement than just the increase in the number of filled beds, however: it’s a sign of how the hospital is turning a corner.
“We are moving further and further away from disaster,” he said, also noting “I want everybody in the hospital to treat our community well, and I want everyone to treat the hospital well.”






